Dematopathology Decoder Examples
Below are three case examples of standard skin pathology report text accompanied by analysis results from the Dermatopathology Decoder.
Case #1 : 62 year old, male, left forearm excision with ulcerated melanoma.
Pathology Report Text
"HISTOPATHOLOGY Solar keratosis left forearm.MACROSCOPY Container unlabelled as to site - An oval piece of skin 14 x 11 x 5mmbearing a cream macule 8 x 6mm. 4TS, all in. 1 block. scaMICROSCOPY@ESections show a variable crust of polymorphs, fibrin and keratoticmaterial overlying focally ulcerated epidermis. There are variablysized nests of atypical melanocytes lining the basal epidermis andextending into the dermis widely to reach the dermis but not into thesubcutaneous fat. There is focal pagetoid invasion by the epidermis bythe atypical melanocytes. The atypical melanocytes show minimalpigmentation and are composed of large pleomorphic cells with round tooval nuclei, prominent nucleoli with granular to vacuolated cytoplasm.There is a variable degree of lymphocytic infiltrate through thelesion. Intravascular tumour is not identified in the sections. Thelesion extends to a depth of 1.85mm and is a *****'s level IV malignantmelanoma. The lesion extends within 0.5mm of a lateral cut margin.A wider excision is advised.The tumour was submitted for immunoperoxidase stains and the tumourcells are positive for Melan-A and S100. The tumour is negative forcytokeratins Cam 5.2, AE1/AE3.SYNOPTIC REPORT - MALIGNANT MELANOMA@{1} DIAGNOSIS: ULCERATED MALIGNANT MELANOMA INVASIVE WITH ADJACENT SUPERFICIAL AA SPREADING COMPONENT. SITE: LEFT FOREARM CLARK LEVEL: IV BRESLOW THICKNESS: 1.85mm ULCERATION: PRESENT ALYMPHOVASCULAR INVASION: ABSENT NEUROTROPISM/DESMOPLASIA/SATELLITES: ABSENT FEATURES OF REGRESSION: ABSENT ASSOCIATED NAEVUS (TYPE): ABSENT MARGINS: THE NEAREST MARGIN IS THE DEEP MARGIN WHICH IS 0.3mm CLEAR WHILE A THE LATERAL MARGINS ARE 0.5mm CLEAR ARECOMMENDATION: WIDER EXCISION IS ADVISED. {2} SUMMARY DIAGNOSIS@XCISION OF LESION, LEFT FOREARM A - ULCERATED INVASIVE MALIGNANT MELANOMA WITH ADJACENT SUPERFICIAL AA SPREADING COMPONENT, CLARK'S LEVEL IV BRESLOW THICKNESS 1.85mm. AA WIDER EXCISION ADVISED. Reported by Dr. *****************: ************** **********"
Case #1 Dematopathology Decoder Summary (click to expand)
Analysis Results:
| # | Question | Result | Details |
|---|---|---|---|
| 1 | Skin Specimen? | Yes | The report mentions an oval piece of skin from the left forearm. |
| 2 | Number of Specimens? | 1 | The report refers to a single piece of skin. |
| 3 | Number of Pathologists? | 1 | The report was signed off by a single pathologist. |
| 4 | Contradictory Information? | No | The report is consistent in its findings. |
| 5 | Probability of Malignant Melanoma? | 5/5 | The report definitively identifies the presence of malignant melanoma. |
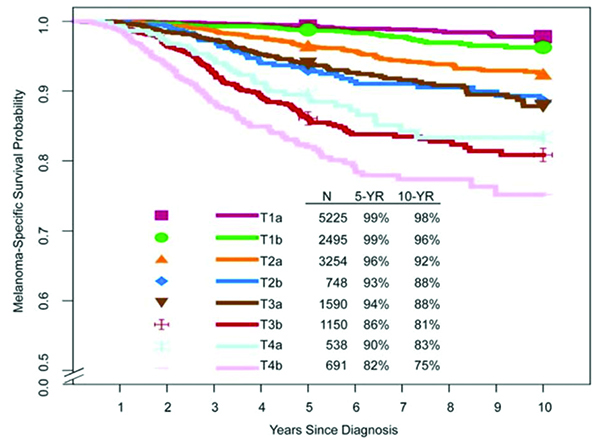
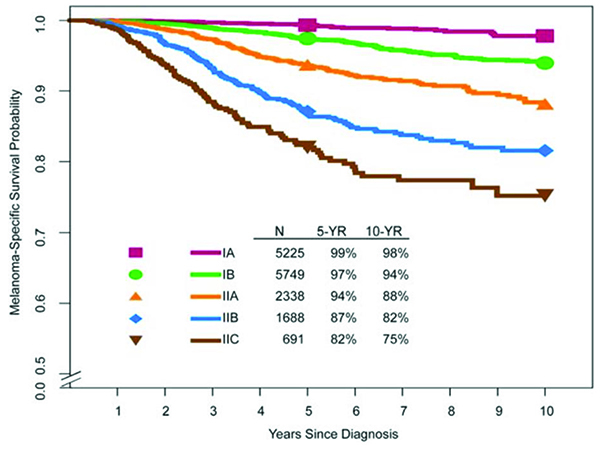
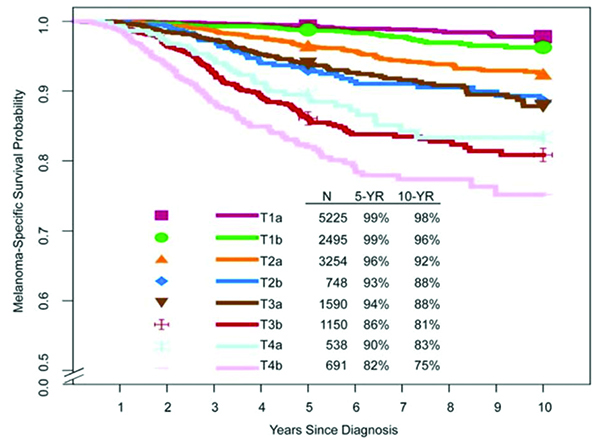
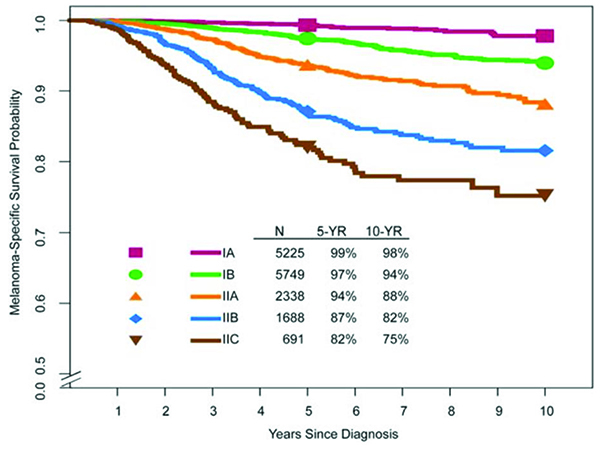
| 6 | Pathology Stage? | Stage II | Based on the Breslow thickness of 1.85mm, the melanoma is likely at Stage II. |
| 7 | Likely ICD10 Code(s)? | C43.9 | This code is for malignant melanoma of skin, unspecified. |
| 8 | Recommendations? | Yes | A wider excision is advised. |
| 9 | Level of Diagnostic Ambiguity? | 0/5 | The report language is clear and unambiguous. |
| 10 | Additional Pathologist Review Needed? | No | The diagnosis is clear, and no further review is necessary. |
| 11 | Melanoma Genomic Test Needed? | No | The diagnosis is clear, and no further testing is necessary. |
Melanoma Analysis Results:
| # | Question | Result | Details |
|---|---|---|---|
| 1 | Breslow Thickness? | 1.85mm | Stated in the report. |
| 2 | Radial diameter? | Not stated | Not mentioned in the report. |
| 3 | Clark Level? | IV | Stated in the report. |
| 4 | Ulceration? | Present | Stated in the report. |
| 5 | Mitotic Rate? | Not stated | Not mentioned in the report. |
| 6 | Lymphovascular Invasion? | Absent | Stated in the report. |
| 7 | Tumor-infiltrating lymphocytes? | Not stated | Not mentioned in the report. |
| 8 | Desmoplasia? | Absent | Stated in the report. |
| 9 | Microsatellites? | Absent | Stated in the report. |
| 10 | Summary of any IHC performed? | Melan-A,S100,Cam 5.2,AE1/AE3 | Positive for Melan-A, a marker often used to confirm a diagnosis of melanoma. Positive for S100, another marker often used to confirm a diagnosis of melanoma. Negative for Cam 5.2, indicating that the tumor is not of epithelial origin. Negative for AE1/AE3, further indicating that the tumor is not of epithelial origin. |
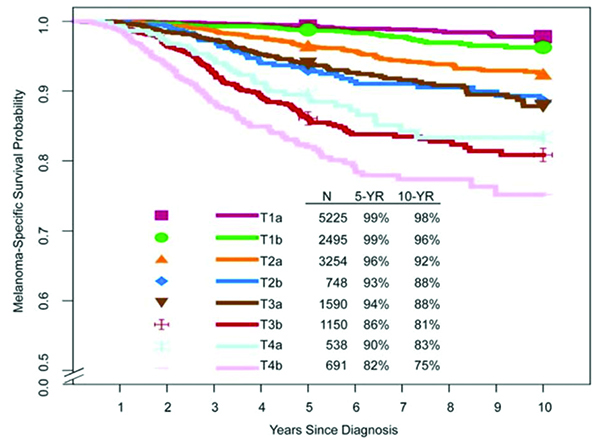
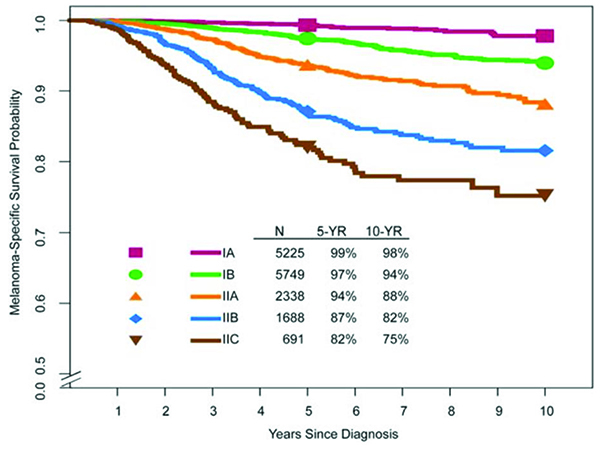
Melanoma prognosis
The prognosis for this patient would likely be fair to good, given that the melanoma is at Stage II and there is no evidence of lymphovascular invasion or desmoplasia. However, the presence of ulceration may negatively impact the prognosis.
Case Summary and Potential Next Steps
The histopathology report describes a skin specimen from the left forearm, which has been diagnosed as an ulcerated malignant melanoma with a Breslow thickness of 1.85mm. The melanoma is likely at Stage II, and a wider excision of the lesion is recommended. This recommendation is based on the clear and unambiguous diagnosis provided in the report.
Report Metadata:
| Detail | Response |
|---|---|
| Specimen id: | Not stated |
| Date: | Not stated |
| Pathologist name: | Not stated |
| Patient name: | Not stated |
Case #2 : 40 year old Male, right calf excision with atypical compound melanocytic lesion.
Pathology Report Text
"Skin (R) calf.MACROSCOPIC DESCRIPTION Labelled "(R) calf".Specimen consists of an ellipse of skin measuring 13x7mm to a depth of2mm. On the surface is a pigmented papule measuring 5x4mm. Lesion allprocessed. 2T sections on 1 block. (**/**)MICROSCOPIC DESCRIPTION@EESections of skin show mildly keratotic epidermis and dermis with acompound atypical melanocytic lesion. There is atypical junctionalmelanocytic cells with nest formation and focal lentiginous activity andsuperficial spreading melanocytic cells could be seen on H&E stain, someof them reaching the granular layer. Underlying dermal melanocytic cellsappear epithelioid and show atypical nuclear features, includingprominent nucleoli and the features of maturation are not clearly seen.Mitotic activity is noted, few in the lwer one third of the lesion (upto1/mm2). The dermal lesion is 0.73mm in thickness and 1.6mm clear of theclosest peripheral margin. The junctional component extends beyond thedermal melanocytes and 0.3mm ******** vascular invasion or neurotropism is noted.The overall appearances are those of an atypical compound melanocyticlesion.I have discussed this case with my **********, and they have agreed thatthis is a challenging one.Many of us felt that features are in favour of a melanoma.Further report to follow.@ECONCLUSION@ESKIN, RIGHT CALF, EXCISION-- ATYPICAL COMPOUND MELANOCYTIC LESION (SEE TEXT).@ AAReported by Dr xxx xx(Direct Phone No. *********) 29/11/2012 SYNOPTIC REPORT FOR CUTANEOUS MALIGNANT MELANOMA. Site:Diagnosis:Type/Classification:Predominant cell type:Breslow thickness:Clark Level:Ulceration present:Dermal mitotic count: (per mm2)Vascular space invasion:Perineural invasion:Microsatellites:Features of regression: - Tumour infiltrating lymphocytes (TILS):- Capillary proliferation:- Loss of rete ridges:- Fibrosis:Associated naevus (include type):Closest peripheral margin to in-situ component:Closest peripheral margin to invasive component:Distance to deep margin:"
Case #2 : Dematopathology Decoder Summary
Analysis Results:
| # | Question | Result | Details |
|---|---|---|---|
| 1 | Skin Specimen? | Yes | The report mentions 'Sections of skin show mildly keratotic epidermis and dermis with a compound atypical melanocytic lesion.' |
| 2 | Number of Specimens? | 1 | The report mentions one specimen from the right calf. |
| 3 | Number of Pathologists? | 2 | The report mentions the primary pathologist and another with whom the case was discussed. |
| 4 | Contradictory Information? | No | The report does not contain any contradictory information. |
| 5 | Probability of Malignant Melanoma? | 4/5 | The report mentions 'Many of us felt that features are in favour of a melanoma.' |
| 6 | Pathology Stage? | Stage I | The Breslow thickness of the lesion is 0.73mm, which suggests a Stage I melanoma. |
| 7 | Likely ICD10 Code? | C43.9 | This is the code for malignant melanoma of skin, unspecified. |
| 8 | Specific Recommendations? | No | The report does not contain any specific recommendations. |
| 9 | Diagnostic Ambiguity? | 3/5 | The report mentions 'this is a challenging one', indicating moderate ambiguity. |
| 10 | Additional Pathologist Review? | Yes | Given the moderate level of ambiguity, an additional review could be beneficial. |
| 11 | Melanoma Genomic Test? | Yes | Given the moderate level of ambiguity, a genomic test could help resolve diagnostic ambiguity. |
Melanoma Analysis Results:
| # | Question | Result | Details |
|---|---|---|---|
| 1 | Breslow Thickness? | 0.73mm | Stated in the report. |
| 2 | Radial diameter? | Not stated | Not provided in the report. |
| 3 | Clark Level? | Not stated | Not provided in the report. |
| 4 | Ulceration? | Not stated | Not provided in the report. |
| 5 | Mitotic Rate? | 1/mm2 | Stated in the report. |
| 6 | Lymphovascular Invasion? | No | No vascular invasion or neurotropism is noted in the report. |
| 7 | Tumor-infiltrating lymphocytes? | Not stated | Not provided in the report. |
| 8 | Desmoplasia? | Not stated | Not provided in the report. |
| 9 | Microsatellites? | Not stated | Not provided in the report. |
| 10 | Summary of any IHC performed? | No IHC stains mentioned | The report does not provide information on IHC stains |
Melanoma prognosis
Given the Breslow thickness of 0.73mm and a mitotic rate of 1/mm2, the prognosis for this patient is generally good, as these factors suggest a Stage I melanoma. However, the exact prognosis would depend on several other factors not provided in the report, such as the presence of ulceration, lymphovascular invasion, and patient's overall health.
Case Summary and Potential Next Steps
The pathology report describes an atypical compound melanocytic lesion from the right calf that shows features suggestive of a melanoma. The lesion has a Breslow thickness of 0.73mm, indicating a likely Stage I melanoma. Given the moderate level of diagnostic ambiguity, it would be beneficial to have an additional pathologist review the case and consider conducting a melanoma genomic test to help resolve any diagnostic uncertainty.
Report Metadata:
| Detail | Response |
|---|---|
| Specimen id: | Not provided |
| Date: | Not provided |
| Pathologist name: | Dr xxx xx |
| Patient name: | Not provided |
Case #3 : 84 year old female, multiple lesions excised, melanoma identified.
Pathology Report Text
"1) Left proximal anterior tibia ? ***. 2) Left lat ant tib ? ***. 3)Left prox med malleolus ? ***.MACROSCOPY "Left proximal anterior tibia" - A core of skin 2mm in diameter x 2mmin depth. All in.2) "Left lateral anterior tibia" - A core of skin 2mm in diameter x 4mmin depth. All in.3) "Left proximal malleolus" - A core of skin 2mm in diameter x 3mm indepth. All in. rtMICROSCOPY@E1) The punch biopsy shows hyperkeratotic squamous intraepidermalcarcinoma.2) The biopsy shows an atypical compound melanocytic lesion compatiblewith malignant melanoma, NOS. The in-situ component consists of singleatypical lentiginous melanocytic proliferation. The invasive componentextends to a depth of at least 1.25mm to reticular dermis. The lesiondisplays mixed epithelioid and spindled morphology. There is a mildlymphocytic infiltrate. The biopsy is right through the lesion.Appropriate wider excision recommended.3) A well differentiated squamous cell carcinoma involves thefull-thickness of the biopsy.SUMMARY DIAGNOSIS@EE1) LEFT PROXIMAL ANTERIOR TIBIA, PUNCH BIOPSY - INTRAEPIDERMAL CARCINOMA. 2) LEFT LATERAL ANTERIOR TIBIA, PUNCH BIOPSY A - MALIGNANT MELANOMA, NOS. A - BRESLOW THICKNESS 1.25mm, CLARK LEVEL IV. - *********** WIDER EXCISION RECOMMENDED. 3) LEFT PROXIMAL MEDIAL MALLEOLUS, PUNCH BIOPSY - SQUAMOUS CELL CARCINOMA. AReported by Dr. xx, **, **********: **********"
Case #3 : Dematopathology Decoder Summary
Analysis Results:
| # | Question | Result | Details |
|---|---|---|---|
| 1 | Is the specimen skin? | Yes | The report refers to a 'core of skin' and 'punch biopsy', indicating the specimen is skin. |
| 2 | Number of specimens reviewed? | 3 | The report mentions three different locations from which the specimens were taken. |
| 3 | Number of pathologists? | 1 | The report is signed off by one pathologist, Dr. **. |
| 4 | Contradictory information? | No | The report provides consistent information about the diagnoses for each specimen. |
| 5 | Probability of malignant melanoma? | 5/5 | One of the specimens is explicitly diagnosed with malignant melanoma. |
| 6 | Pathology stage? | Stage II | The Breslow thickness of 1.25mm and Clark Level IV suggest a Stage II melanoma. |
| 7 | ICD10 code(s)? | C43.9, C44.9, C44.0 | C43.9 for malignant melanoma, C44.9 for intraepidermal carcinoma, and C44.0 for squamous cell carcinoma. |
| 8 | Specific recommendations? | Yes | The report recommends a wider excision for the malignant melanoma. |
| 9 | Level of diagnostic ambiguity? | 0/5 | The report provides clear and definitive diagnoses for each specimen. |
| 10 | Need for additional pathologist review? | No | Given the definitive language and clear diagnoses, another pathologist review is unlikely to provide additional clarity. |
| 11 | Need for melanoma genomic test? | No | The diagnosis of malignant melanoma is clear, and a genomic test is unlikely to provide additional information. |
Melanoma Analysis Results:
| # | Question | Result | Details |
|---|---|---|---|
| 1 | Breslow Thickness? | 1.25mm | Stated in the report. |
| 2 | Radial diameter? | Not stated | Not provided in the report. |
| 3 | Clark Level? | IV | Stated in the report. |
| 4 | Ulceration? | Not stated | Not provided in the report. |
| 5 | Mitotic Rate? | Not stated | Not provided in the report. |
| 6 | Lymphovascular Invasion? | Not stated | Not provided in the report. |
| 7 | Tumor-infiltrating lymphocytes? | Mild | A mild lymphocytic infiltrate is mentioned in the report. |
| 8 | Desmoplasia? | Not stated | Not provided in the report. |
| 9 | Microsatellites? | Not stated | Not provided in the report. |
| 10 | Summary of any IHC performed? | No IHC stains mentioned | The report does not provide information on IHC stains |
Melanoma prognosis
Given the Breslow thickness of 1.25mm and Clark Level IV, the prognosis for this patient would be considered moderate. The recommended wider excision could potentially improve the prognosis if all of the malignant tissue is successfully removed.
Case Summary and Potential Next Steps
The pathology report indicates that three skin biopsies were taken, each with a different diagnosis: intraepidermal carcinoma, malignant melanoma, and squamous cell carcinoma. The melanoma has a Breslow thickness of 1.25mm and is at Clark Level IV, suggesting a stage II melanoma. The pathologist recommends a wider excision for the melanoma. Given these findings, the next steps should include a wider excision of the melanoma as recommended, as well as appropriate treatment for the intraepidermal and squamous cell carcinomas.
Report Metadata:
| Detail | Response |
|---|---|
| Specimen id: | Not stated |
| Date: | Not stated |
| Pathologist name: | Dr. ** |
| Patient name: | Not stated |